24 weeks 5 days, 890 grams (2lb)
Life in our house was noisy, crazy and busy. I was in my second trimester with our third baby, I was still trying to come to terms with how a third child could ever survive alongside his two boisterous brothers (2 and 4yrs old) but took comfort that there were still nearly 4 months to go… or so I thought!
One late November morning, 2012, I had a routine follow-up scan to get the missing shot of our baby’s face (this was the 4th attempt), obtaining the face shot quickly paled into insignificance when the sonographer saw how low my waters were; the light bleeding that I’d been having for the previous 2 weeks had been masking ruptured membranes and infection (which came first we’ll never know). A gynaecologist appointment was made for that afternoon, I had an inkling that perhaps my husband should make it to this appointment, and he dutifully took time off work to meet me and my midwife there. Within 10 minutes of arriving I had an enormous bleed and began contractions within minutes. The Obstetrician was on his way and the Neonatal team was promptly given the code red, this baby was coming! I transitioned into second stage labour so quickly that there was no time for steroids or surfactant to help prepare his immature lungs. There was a constant flurry of activity around me, the room was suddenly full of people and all I could think about was how I wasn’t even remotely prepared to go through the labour pains that were suddenly storming my body! Within 40 minutes I went from ‘pregnant with the possibility of ruptured membranes’ to ‘Sheesh, there’s our baby! I guess we should start thinking about a name…”
We were naive, I knew babies were viable after 23 weeks so I wasn’t as worried as perhaps I should have been. We live in Palmerston North, and thank God that I went into labour in the only place in the city that would have supported our baby’s life; but it wasn’t a place that could get him through the next couple of months.
Our 2 lb (890g) baby boy was wired up, lined in and plugged into beeping, flashing, life-saving equipment. Wrapped in plastic to protect his fragile skin, his face was flat and remarkably undefined. His bright red, translucent fingers wrapped perfectly around the tip of my index finger, tiny, intricate, fearfully and wonderfully made. His eyes were fused shut but moved rapidly as he slept. A few hours of preparation led to a helicopter ride with his Dad to his new home in Wellington NICU, I followed the next day. It was a tearful goodbye to our older boys, they too had no warning that their life would be totally turned upside down. We are forever grateful to our parents and siblings for filling in for us where we weren’t able to, to do this without family support would be so, so hard.
Life at NICU was transforming. We were put through a crash course in human biology and how to care for our NICU baby. Every day brought new challenges, concerns or celebrations. We watched our baby writhe in pain and sleep in blissful ignorance. We read his charts and followed his progress. We became vigilant and paranoid around hygiene and germs. My life was organised around the clock, 3 hourly expressing, 6 hourly cares, 2-3 hour long cuddles – on the good days, saying good night and leaving my baby in the care of the nurses until morning. Day in day out. But he grew. He started tolerating. He improved. And eventually the day finally came after two months where he was well enough to send home to Palmerston North Hospital, such a happy day!
At nearly 34 weeks (gestational age) Eli was flown back to Palmerston North Hospital, what a huge transition this was! In Wellington I had grown used to being just across the road at the Ronald McDonald House. If there was an emergency I could be there in minutes, it was easy to get there for all his cares, and late evening visits were quite feasible. Now at home, I was so thankful to be available to my other two boys, but it was also extremely exhausting; my time and energy was stretched very thin! A trip to hospital required babysitters and took a lot longer, I was driving to and from hospital around four times a day after breastfeeding was established so there wasn’t much time for anything else! Family, friends and Church family were such a wonderful support; we had people offering to clean the house, tidy up the garden, mow the lawns, cook us dinner and a loyal few who would drop everything to support me with babysitting when I had to zip up for the next lot of cares. These people were invaluable, if you’re in the journey, let people help you and don’t be afraid to ask for help; people I barely knew were only too happy to do their bit in supporting us, sometimes they just needed an invitation.
Understandably, Neonates in Palmerston North was a different ship. There were still the basic hygiene steps but things were very different to what I’d grown used to in Wellington. Nurses and specialists did things differently, they saw him at the age he was rather than what he had been. Slowly we had to remove the layers of cotton wool and expose our baby to the big bad world (within the confounds of an incubator and locked Neonatal ward!). Day by day, the change became easier, priorities changed and transitions become inevitable. It was wonderful to start the process of breastfeeding at 34 weeks (gestational age), and around 37 weeks he came off oxygen and his feeding tube soon followed.
It is hard to know the toll it took on our other two children, I was no longer doing the role I had been doing, other people were taking them places and interacting with them, and they were spending considerable time in other homes. Our 4 year old’s behavior was difficult to manage at the best of times, but after he told another Mum at Playcentre that “Mum’s never coming back” we realised how significant this upheaval had been on him. Remember to talk openly to you older children as they can make some surprising interpretations out of the situation they’ve been put in.
We returned to Wellington NICU for a bilateral hernia repair where he briefly lapsed back on to oxygen support. After 123 days in hospital (42 weeks g/a) Elias was discharged, free of oxygen support and tubes and with a rather courageous leap, he soon became exclusively breastfed! What a joy it was to take him home, life was able to return to a more reasonable pace, I could enjoy breastfeeding in the comfort of our home, and share more of his cares alongside my husband and family.
Keeping our house free from coughs and colds was near impossible.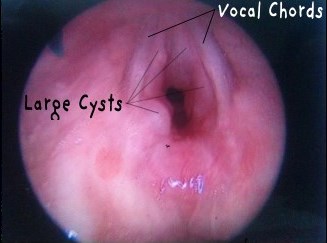 Our oldest had just started school and our second just started preschool, I was not going to consider home schooling! Sure enough Eli got sick too. Thankfully, most of the colds he caught over this year he coped as well as any new born. It wasn’t until he was around 9 months (actual age) that he caught his first bout of croup. A long scary 5 days in hospital led to serious questions being asked. By 11 months (actual age) he was wheezy all the time, and his voice was strained and weak. We were flown up to Starship Hospital to investigate a “mass” under his vocal chords. It turned out his airways were severely restricted by 7 cysts on and around his vocal chords. Cysts like this are common in intubated patients, which he needed 4 times in his early days at NICU. One year on, Eli has undergone 5 procedures to remove these cysts, he now vocalises well, and has a much healthier airway. Although we’ll have a follow up appointment in a year’s time, we are expecting this to be the last of his big hurdles!
Our oldest had just started school and our second just started preschool, I was not going to consider home schooling! Sure enough Eli got sick too. Thankfully, most of the colds he caught over this year he coped as well as any new born. It wasn’t until he was around 9 months (actual age) that he caught his first bout of croup. A long scary 5 days in hospital led to serious questions being asked. By 11 months (actual age) he was wheezy all the time, and his voice was strained and weak. We were flown up to Starship Hospital to investigate a “mass” under his vocal chords. It turned out his airways were severely restricted by 7 cysts on and around his vocal chords. Cysts like this are common in intubated patients, which he needed 4 times in his early days at NICU. One year on, Eli has undergone 5 procedures to remove these cysts, he now vocalises well, and has a much healthier airway. Although we’ll have a follow up appointment in a year’s time, we are expecting this to be the last of his big hurdles!
Elias, now just past his 2nd birthday (corrected age), is an active, happy  and opinionated 2yr old. He runs around, tackles (and is tackled by) his 2 big brothers, climb’s to great heights, follows instructions and communicates effectively (through sign, gestures and a scattering of words), he melts my heart every time he notices someone in tears, he’ll gently pat their head and follow up with a cuddle, if a toy’s been stolen off them, Eli will find another one to bring them. His hands and feet still bear the mark of every cannula he endured, every heel prick he received, faint lines where he wore his leg cast for 2 months and a long dent where his long line was inserted. I look at these with pride; our boy has been through so much, but through all of this, we are forever thankful to the life-giving facilities and expertise that the NICU provided, and the caring and supportive role the Little Miracles Trust played, connecting parents and being a listening ear during this extremely emotional and stressful time. We still keep in touch with a number of parents that shared this NICU journey with us through a Facebook page; I’d highly recommend this if you’re in the middle of your NICU journey, these parents can truly understand the journey you’re on, we share in our celebrations and are supported through our trials. Thanks to God, and these outstanding facilities, we now have a precious, healthy little boy that warms our heart daily.
and opinionated 2yr old. He runs around, tackles (and is tackled by) his 2 big brothers, climb’s to great heights, follows instructions and communicates effectively (through sign, gestures and a scattering of words), he melts my heart every time he notices someone in tears, he’ll gently pat their head and follow up with a cuddle, if a toy’s been stolen off them, Eli will find another one to bring them. His hands and feet still bear the mark of every cannula he endured, every heel prick he received, faint lines where he wore his leg cast for 2 months and a long dent where his long line was inserted. I look at these with pride; our boy has been through so much, but through all of this, we are forever thankful to the life-giving facilities and expertise that the NICU provided, and the caring and supportive role the Little Miracles Trust played, connecting parents and being a listening ear during this extremely emotional and stressful time. We still keep in touch with a number of parents that shared this NICU journey with us through a Facebook page; I’d highly recommend this if you’re in the middle of your NICU journey, these parents can truly understand the journey you’re on, we share in our celebrations and are supported through our trials. Thanks to God, and these outstanding facilities, we now have a precious, healthy little boy that warms our heart daily.
You can find Eli’s story on the walls of the Wellington NICU: